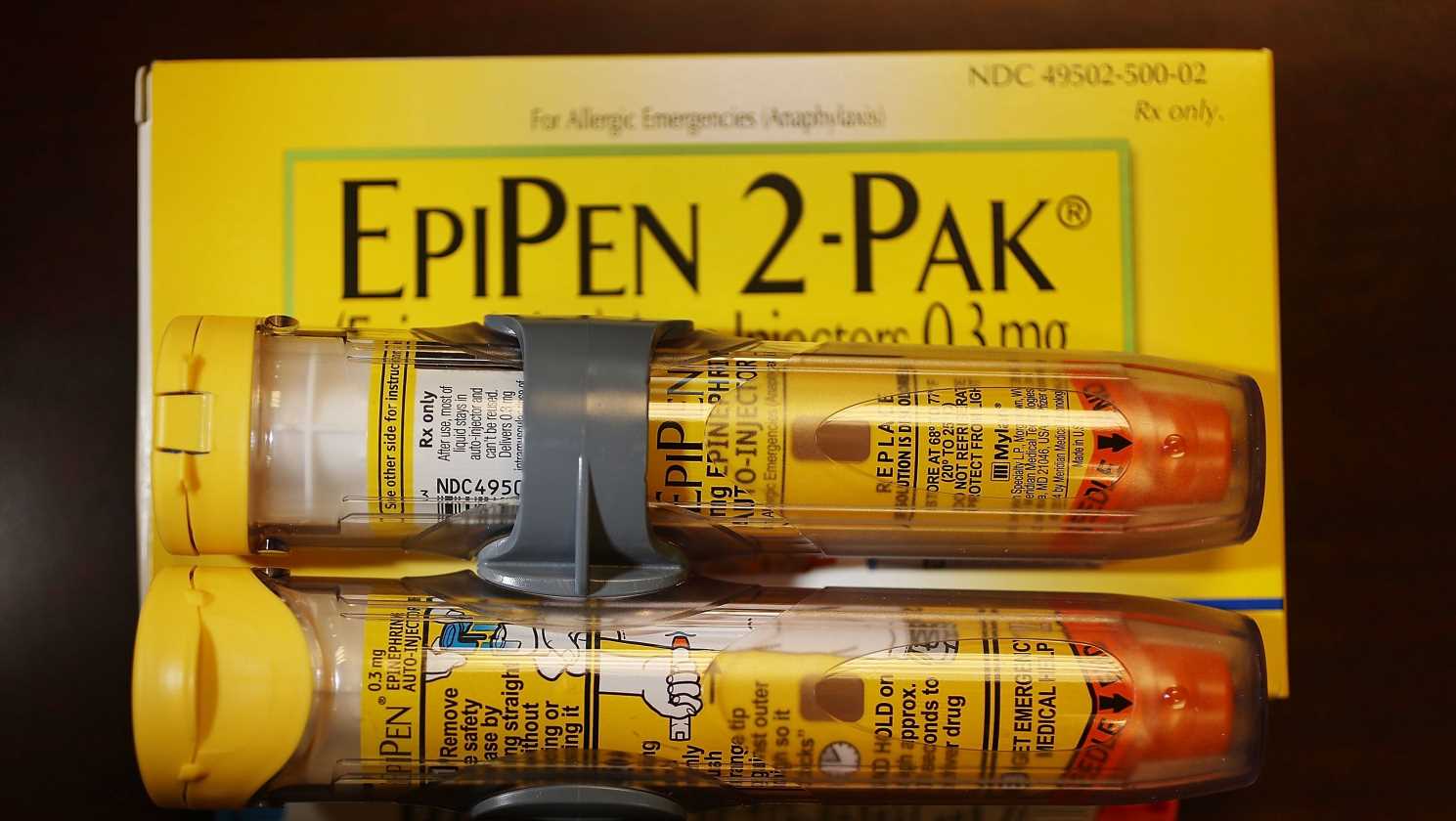
An Illinois law will take effect Jan. 1, 2020 requiring companies offering health insurance policies to pay for medically necessary epinephrine injectors for minors. (Photo: Joe Raedle, Getty Images)
This week Illinois became the first state to shift the burden of paying for a potentially life-saving shot of an epinephrine injection for children from parents to insurance companies.
Illinois Gov. JB Pritzker signed a law that would require companies offering health insurance policies in the state to pay for medically-necessary epinephrine injectors for cases of severe allergic reactions for those 18 and younger. House Bill 3435 takes effect Jan. 1.
The Allergy and Asthma Network confirmed in an email to USA TODAY that Illinois is the first state to require insurance companies pay for injectors.
Pritzker tweeted that the legislation is “a big step forward in protecting our children and families.”
Parents can only hope Illinois serves as an example for other states as they struggled last year with finding EpiPens, by far the largest the largest provider of the epinephrine injection system, and paying for them amid rising costs.
“As a parent whose kid needs an epipen (which “expires” every six months) at school, camp, and grandmas, this is huge,” tweeted @mbenko23.
An epinephrine injector, used during an anaphylactic attack, delivers a dose of epinephrine, or adrenaline that minimizes swelling and opens airways.
Illinois State Senator Julie Morrison said no child should suffer because they can’t afford an EpiPen. The cost of the EpiPen jumped from $57 in 2007 to about $500 in 2016.
“With steady increases in food allergies and other serious allergic conditions, families are relying on EpiPens more than ever before,” Morrison said in a statement. “We should be doing everything we can to expand access to affordable lifesaving drugs and medicines. No child with a serious allergy should be without an epinephrine injector because they cannot afford one.”
Source: Read Full Article