Fertility drugs used in IVF do NOT increase the risk of women developing breast cancer, study finds
- Scientists perform ‘largest study to date’ on fertility drugs and breast cancer risk
- Drugs used to release eggs ‘do not increase the risk of developing breast cancer’
- Fertility medications taken by women include gonadotropins and clomiphene
Drugs used during fertility treatments to release eggs do not increase the risk of developing breast cancer, a study shows.
Researchers from King’s College London analysed studies involving 1.8 million women undergoing fertility drug treatments.
The women, all of whom had no previous history of breast cancer, were followed up in studies for an average period of 27 years.
Researchers found they showed ‘no significant increase’ in the risk of developing breast cancer compared to those who hadn’t taken the drugs.
The research is the largest study to date assessing whether commonly used fertility drugs are a cancer risk for women, researchers say.
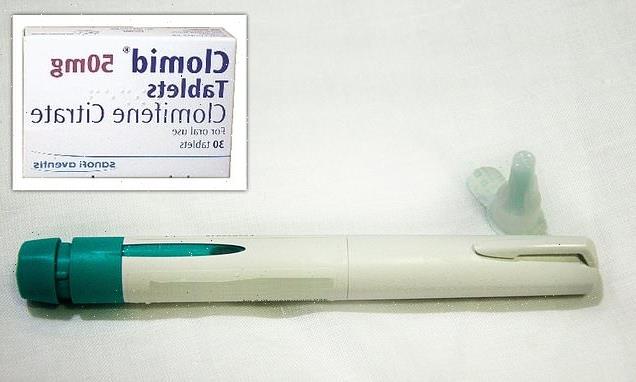
Pictured, syringe and needle to inject gonadotropins, a fertility medication. No significant increase in the risk of breast cancer was found with the use of gonadotropins or clomiphene citrate, alone or in combination, the King’s College London team reveal
‘Fertility treatment can be an emotional experience,’ said study author Dr Yusuf Beebeejaun from King’s College London.
‘Patients often ask us if taking ovarian stimulating drugs will put them at increased risk of developing cancers, including breast cancer.
‘To answer that important clinical question, we undertook this review that reports data from nearly 2 million people.’
Fertility drugs to stimulate ovaries to release eggs have been used to treat infertility since the early 1960s.
All the women within the study used either two types of ovulation stimulation medication, or a combination of both – clomiphene and gonadotrophins.
Both types of drug are marketed worldwide under a variety of brand names.
Gonadotrophins are hormone agents that can be given in an injection to stimulate a woman’s ovaries to produce follicles, which contain an oocyte (egg).
Researchers addressed the association between the use of ovarian stimulation drugs (pictured in stock image) and the risk of developing breast cancer
WHAT IS IVF?
In vitro fertilisation (IVF) is a technique to help people with fertility problems have a baby.
It is the process of sperm fertilising an egg outside the body.
During IVF, an egg is removed from the woman’s ovaries and fertilised with sperm in a laboratory.
The fertilised egg, called an embryo, is then returned to the woman’s womb to grow and develop.
It can be carried out using your eggs and your partner’s sperm, or eggs and sperm from donors.
Source: NHS
Clomiphene, a synthetic chemical that’s taken orally, binds to estrogen receptors in the brain and boosts levels of follicle-stimulating hormone (FSH), which itself is a type of gonadotrophin.
Both clomiphene and gonadotrophins are used as part of an in vitro fertilisation (IVF) treatment to stimulate ovaries.
IVF involves stimulating a patient’s ovarian cycle, extracting eggs from their ovaries, fertilising them with sperm in a laboratory and then transferring the embryo into the womb to develop.
‘While IVF is a process, ovarian stimulation is the first and most important part of the process,’ Dr Beebeejaun told MailOnline.
‘The use of the agents that were looked within this review at are the medications that women will use to stimulate their ovaries to produce more eggs.
‘These eggs will then be retrieved and fertilised and embryos transferred, as part of the entire IVF process.’
The problem is that drugs that are used to stimulate the ovaries increase oestrogen hormone production and can act on breast cells.
There has been concern that this could turn the cells cancerous, which has led to an uncertainty about the potential risk of infertility drugs causing breast cancer.
The researchers’ review, published today in the journal Fertility and Sterility, looked at studies from 1990 to January 2020.
Women of all reproductive ages were included and followed up for an average of 27 years following their fertility treatment.
Researchers found no significant increase in breast cancer risk for women exposed to treatment compared to untreated women, both fertile and infertile.
Clomid, also known as clomiphene citrate, is an oral fertility drug
No significant increase in the risk of breast cancer was found with the use of clomiphene citrate or gonadotropins, alone or in combination.
‘Our study showed that the use of drugs to stimulate ovaries in fertility treatment did not put women at increased risk of breast cancer,’ said Dr Sesh Sunkara, senior-author of the paper, from King’s College London.
‘This study provides the evidence needed to reassure women and couples seeking fertility treatments.’
Dr Kotryna Temcinaite at UK charity Breast Cancer Now, has called for more research into what factors do contribute to someone’s risk of developing breast cancer.
‘Previously it was unclear whether fertility drugs affect breast cancer risk, and we do receive calls to our Helpline from women who are concerned that their breast cancer has been caused by fertility treatment,’ said Dr Temcinaite, who was not involved in the new study.
‘While this analysis of existing published studies does provide welcome reassurance that fertility treatment is unlikely to increase breast cancer risk, further long-term and detailed studies are now needed to confirm these findings.’
HOW DOES IVF WORK?
In-vitro fertilisation, known as IVF, is a medical procedure in which a woman has an already-fertilised egg inserted into her womb to become pregnant.
It is used when couples are unable to conceive naturally, and a sperm and egg are removed from their bodies and combined in a laboratory before the embryo is inserted into the woman.
Once the embryo is in the womb, the pregnancy should continue as normal.
The procedure can be done using eggs and sperm from a couple or those from donors.
Guidelines from the National Institute for Health and Care Excellence (NICE) recommends that IVF should be offered on the NHS to women under 43 who have been trying to conceive through regular unprotected sex for two years.
People can also pay for IVF privately, which costs an average of £3,348 for a single cycle, according to figures published in January 2018, and there is no guarantee of success.
The NHS says success rates for women under 35 are about 29 per cent, with the chance of a successful cycle reducing as they age.
Around eight million babies are thought to have been born due to IVF since the first ever case, British woman Louise Brown, was born in 1978.
Chances of success
The success rate of IVF depends on the age of the woman undergoing treatment, as well as the cause of the infertility (if it’s known).
Younger women are more likely to have a successful pregnancy.
IVF isn’t usually recommended for women over the age of 42 because the chances of a successful pregnancy are thought to be too low.
Between 2014 and 2016 the percentage of IVF treatments that resulted in a live birth was:
29 per cent for women under 35
23 per cent for women aged 35 to 37
15 per cent for women aged 38 to 39
9 per cent for women aged 40 to 42
3 per cent for women aged 43 to 44
2 per cent for women aged over 44
Source: Read Full Article